By Doug Ward
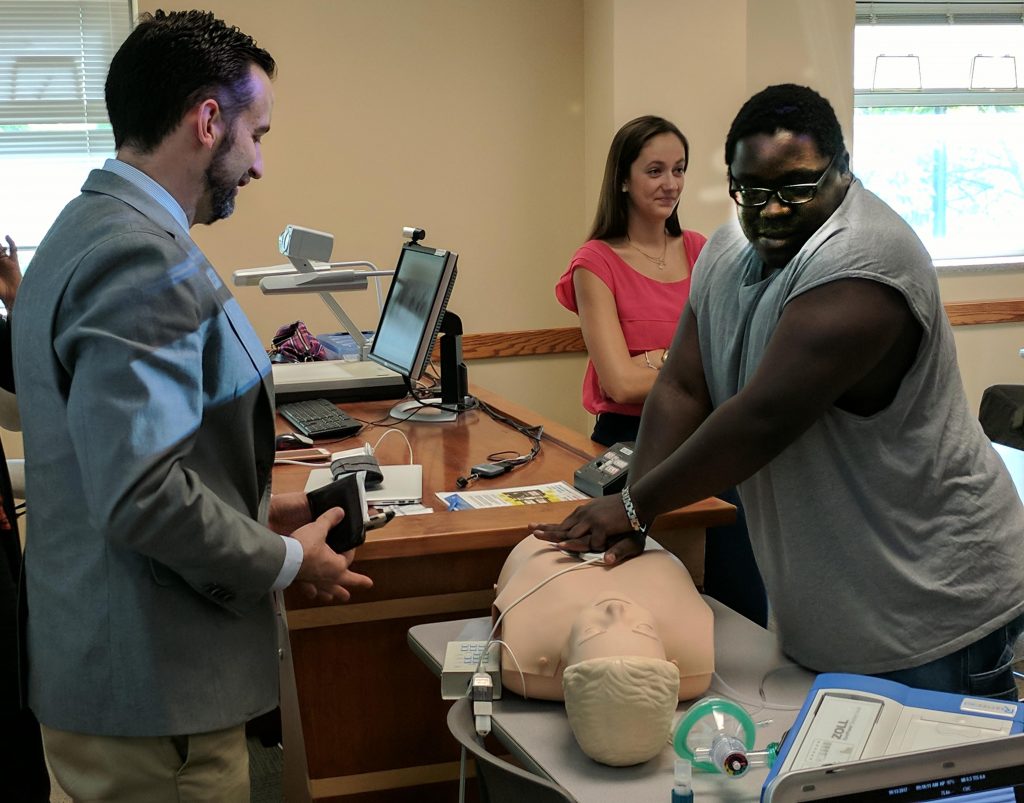
Mannequins have been a part of health care training for decades. As Matt Lineberry of the Zamierowski Institute for Experiential Learning demonstrated recently, though, those mannequins have become decidedly smarter.
Lineberry, director of simulation research, assessment and outcomes at the Zamierowski Institute, spoke with faculty members and graduate students in the educational psychology department in Lawrence, explaining how health care simulation has evolved into highly sophisticated mechanism for gathering data about students’ performance in a variety of medical settings.
The Zamierowski Institute, part of the University of Kansas Medical Center campus, expanded immensely with the opening of the new Health Education Building this fall. It now has spaces where students practice emergency room care, intensive care, operations and other aspects of medicine in realistic settings.
Mannequins are a key part of the learning process. The most sophisticated models, which cost about $100,000, simulate lung sounds, heart sounds, cardiac arrest and a variety of ailments. Students can use ultrasound, feed in catheters, deliver electric shock for cardiac arrest, and administer medication. Software that works with the mannequins gathers dozens of types of data and can even measure the type and dose of medication injected into the simulated patients.

Students also work with actors who take on the roles of “standardized patients” for practicing interpersonal skills. Actors also play family members and colleagues to help doctors and nurses gain experience with interaction. In some cases, the actors wear gear that simulates injuries.
As students work, cameras capture video from many angles. That allows students and instructors to review students’ responses and interactions.
Lineberry said the training had helped cut down on response times in emergencies. He gave an example of a highly trained team of student doctors and nurses who went through a cardiac arrest simulation at the center. For defibrillation to be effective, he said, it must be administered within two minutes of a heart stopping. The team took about seven minutes to administer defibrillation, though. That was eye-opening, Lineberry said, but it demonstrated the value of having hands-on training in a setting where patients aren’t at risk.
The center’s approach has become common not only in health care but in other fields that have adopted augmented and virtual reality. For instance, Case Western Reserve’s use of Microsoft’s Hololens has transformed its teaching of anatomy. Augmented reality has provided architects and engineers new ways of creating and testing prototypes. A digital rendering of Pompeii by researchers at the University of Arkansas has provided new insights into ancient culture. And K-12 schools have found that virtual reality field trips improve students’ retention of information.
Those are just a few of the ways that educators have been using technology to enhance learning and understanding. As with the mannequins, that technology will only grow smarter.
New studio opens in Budig Hall

Doug Ward is the associate director of the Center for Teaching Excellence and an associate professor of journalism. You can follow him on Twitter @kuediting.